慢性腦部疾患病人合併下尿路症狀錄影之錄影尿路動力學分析
江景翔、陳聖復、郭漢崇
佛教慈濟醫療財團法人花蓮慈濟醫院 泌尿部
Videourodynamics analysis of the lower urinary tract dysfunctions in patients with chronic brain disorders
Ching-Hsiang Chiang, Sheng-Fu Chen, Hann-Chorng Kuo
Department of Urology, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation and Tzu Chi University, Hualien, Taiwan
Purpose: Lower urinary tract dysfunction (LUTD) is a common neurological complication in chronic brain disorders. These impact a person’s quality of life, mortality, and the person’s caregiver significantly. This study tried to distinguish the characteristic of LUTD from the findings of video-urodynamic studies (VUDS) in patients with chronic brain lesions as cerebrovascular accident (CVA), Parkinson’s disease (PD) and early dementia.
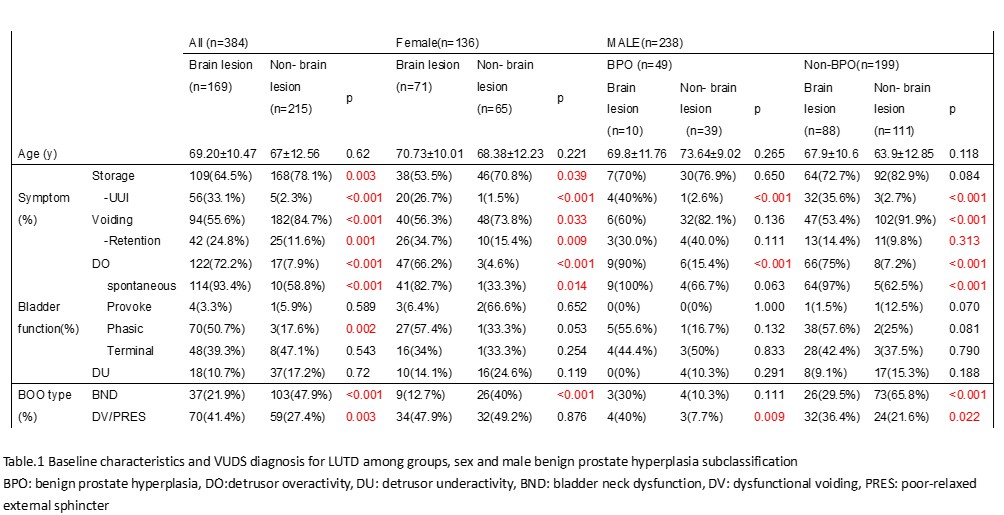
Materials and Methods: This study is a single-center, retrospective review of VUDS database for LUTD from 1997 to 2019 (n=8343). Patients with unavailable past medical history, preexisting urological diseases, spinal cord injury or other neurological diseases were excluded. Total 169 patients with chronic brain lesions history and 215 control patients without known brain insult were enrolled. All enrolled cases had comprehensive chart review included brain disorder type, the period from diagnosis to following LUTD, urodynamic parameter and definite diagnosis of LUTD on VUDS finding.
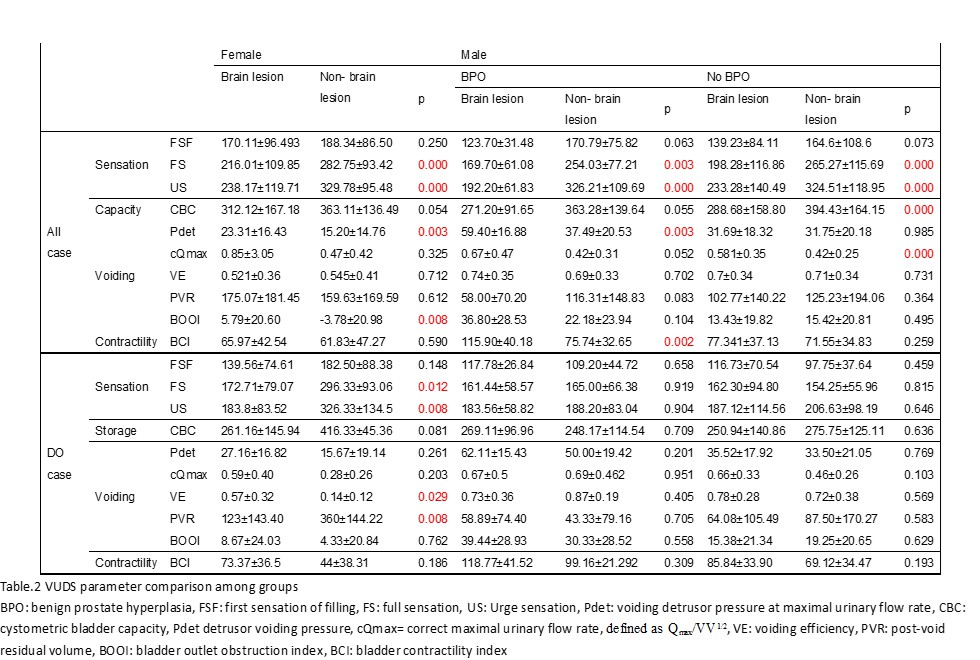
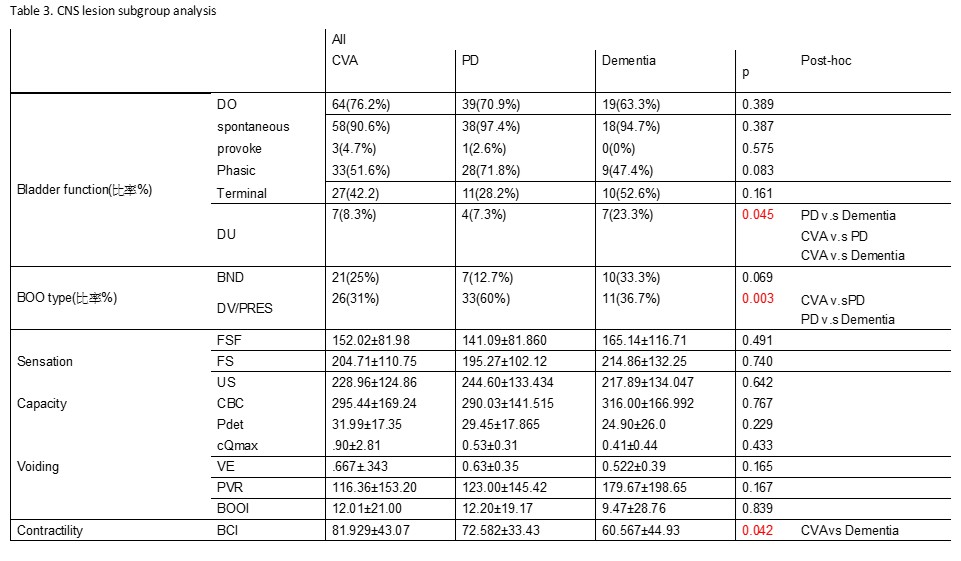
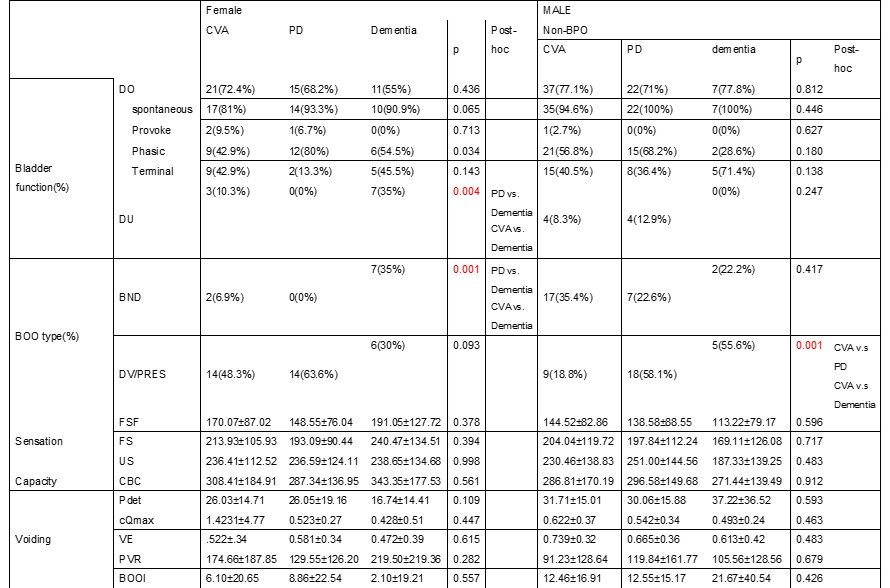
Results: The mean period from brain insult diagnosis to LUTD developed (months) is 61.1 months. Patient with LUTD in non-brain lesion group got higher prevalence of at least one symptom of both storage and voiding (Table.1), while brain lesion group have more severe symptoms (33.1% vs. 2.3% in urge incontinence, p<0.001; and 24.8% vs. 11.6% in retention, p=0.001). Higher rate of detrusor overactivity in brain lesion group (72.2% vs 7.9%, p<0.001), especially spontaneous type DO in female and non-BPO male patient. It also associated with more dysfunctional voiding/poor-relaxed external sphincter (DV/PRES, 41.4% vs 27.4%, p=0.003), and PD cases form the predominant part (60% in PD vs. 31% & 36.7% in CVA and dementia, p= 0.003, respectively). In contrast, more bladder neck dysfunction in control (21.9 vs 47.9%). Patient in brain lesion group had more sensitive bladder as lower volume of full sensation (FS) and urge sensation (US) (Table 2), but only female patient had statistically significant reach in DO subgroup analysis. Brain lesion group female got higher bladder outlet obstruction index (BOOI), poorer voiding efficacy (VE) and larger post-voiding residual volume in DO subgroup.
Conclusions: The real-world VUDS data review of LUTS in chronic brain lesion showed compatible result in DO as previous study, and higher dysfunctional voiding appeared in these cases as the most significant infomation.
附件: