罕見攝護腺刮除術後併發症:嵌頓型腹股溝膀胱憩室疝氣
郭致均1,2、廖俊厚1,3
1天主教耕莘醫院 外科部泌尿科; 2國立台灣大學附設醫院 泌尿部; 3天主教輔仁大學 醫學院
A rare complication after TURP: incarcerated inguinal hernia with bladder diverticulum herniation
Chih-Chun Kuo1,2 and Chun-Hou Liao1,3
1Department of Urology, Cardinal Tien Hospital, 2Department of Urology, National Taiwan University Hospital, National Taiwan University, 3College of Medicine, Fu-Jen Catholic University
Abstract
Inguinal hernias are common conditions routinely been operated worldwide. However, inguinal herniation of the urinary bladder is a rare condition found in only 1-5% of patients. The majority of patient with bladder hernias are asymptomatic and diagnosis is made intraoperatively. Careful physical examination is essential and further image studies may help confirm diagnosis preoperatively. The best management is open surgical repair and possible urinary tract damage during surgery should be recognized and resolved. We report a rare case of post TURP complication, a left-sided inguinal hernia with bladder diverticulum herniation caused by acute urinary retention due to bladder outlet obstruction by blood clots.
Introduction
Inguinal hernias are common conditions routinely been operated worldwide with approximately 20 million hernia surgery annually [1]. However, inguinal herniation of the urinary bladder is a rare condition found in only 1-5% of patients [2-5]. Urinary bladder herniation incidence is higher (about 10%) in obese males, aged over 50 years [4] and is more right-sided [6]. Hernia sac could contain any portion of the bladder including bladder diverticulum, part of the bladder, ureter or the entire bladder. The first case was described in 1951 by Levine [7]. The majority of patient with bladder hernias are symptomatic but some may present with urinary retention or complain of difficulties in urination or double voiding [8]. Careful physical examination is essential and diagnosis is confirmed with ultrasonography, cystography, or computed tomography [5]. However, less than 7% of cases are diagnosed preoperatively [9], most cases are diagnosed intraoperatively [10]. Due to impaired emptying of the bladder, bladder hernias may result in significant urological complications such as obstructive uropathy with consecutive renal failure [11], urinary tract infections and bladder infarctions [12]. Open surgical repair is preferred [2, 4, 8].
The following paper presents a case of patient with incarcerated left-sided inguinal hernia with bladder diverticulum herniation which was caused by acute urinary retention due to bladder outlet obstruction by blood clots, a post TURP complication.
Case report
A 76 years old asian male presented at emergent department due to hematuria for 1 day and subsequently unable to urination with lower abdominal fullness. Tracing back patient’s medical history, he just received transurethral resection of prostate (TURP) 35 days prior to this visit due to benign prostatic hyperplasia with lower urinary tract symptoms. According to operation records, dilated bladder cavity was noted on left lateral wall of bladder during previous surgery, which might indicated to a bladder diverticulum. No hematuria was noted at discharge (post OP day 5), but on and off hematuria noted since one day prior this visit. Patient suffered form acute urinary retention on the day of visit accompanied with lower abdominal pain which mainly focused on left side.
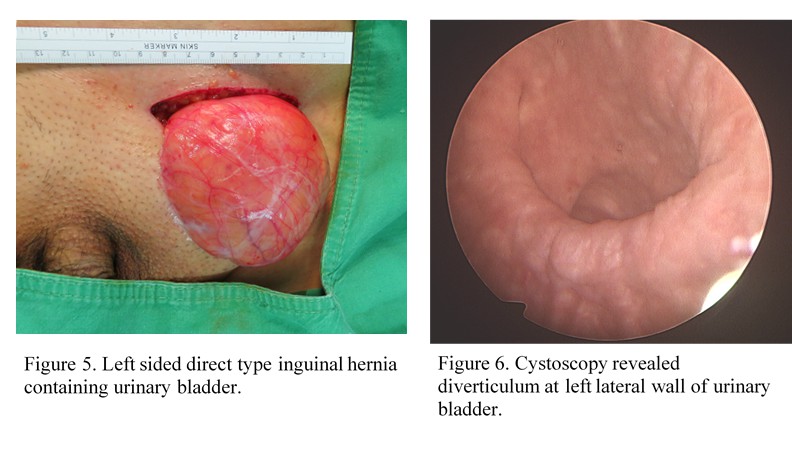
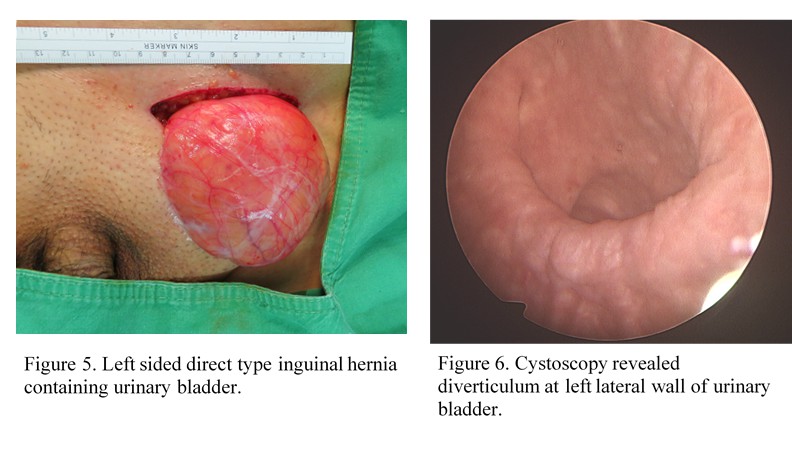
On physical examination, distended urinary bladder with left groin bulging mass were noted. The mass was approximately 10 x 7 cm in size without skin inflammation and painful on palpation. Sonography showed fluid accumulation in the hernia sac, thus bladder rupture due to urinary retention with left inguinal hernia was first considered. Foley catheter was immediately indwelled, some blood clots were evacuated but lower abdominal pain and left inguinal mass persisted. Whole abdominal CT was arranged for differential diagnosis.
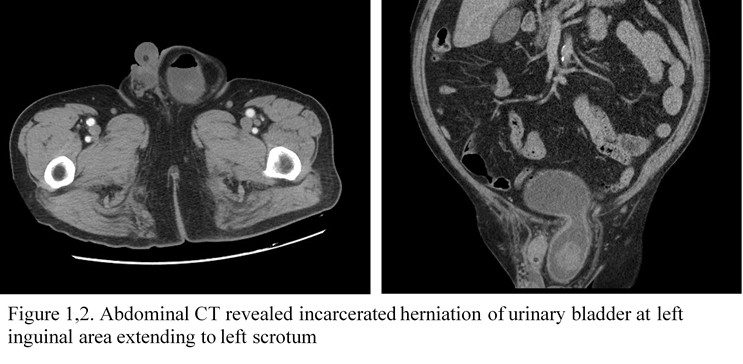
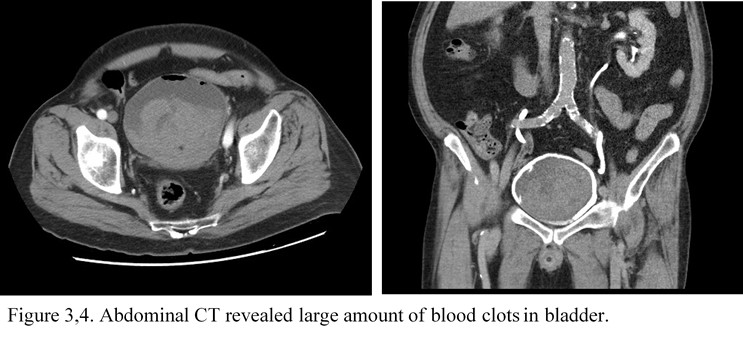
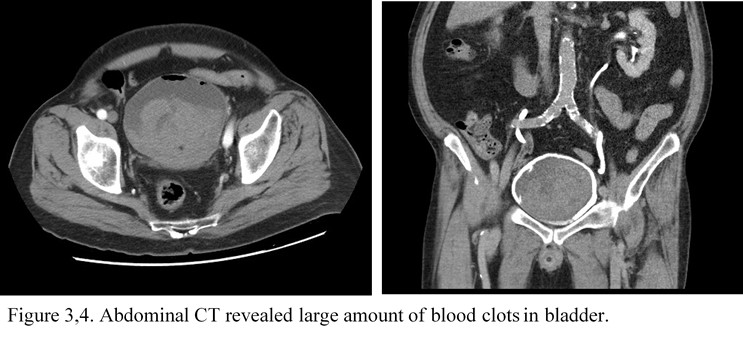
Abdominal CT revealed left inguinal hernia with partial bladder herniation, no bowel loops were noted in the hernia sac (Fig. 1,2). Large amount of blood clots were noted both in the bladder and in herniated bladder (Fig. 3,4).
Patient was admitted to Urology ward and operated on the same day.
Rigid cystoscopy revealed large amount of blood clots in bladder with a bulging mass compressing from left side. Due to poor device mobility, blood clot evacuation was partially performed and converted to open hernia repair.
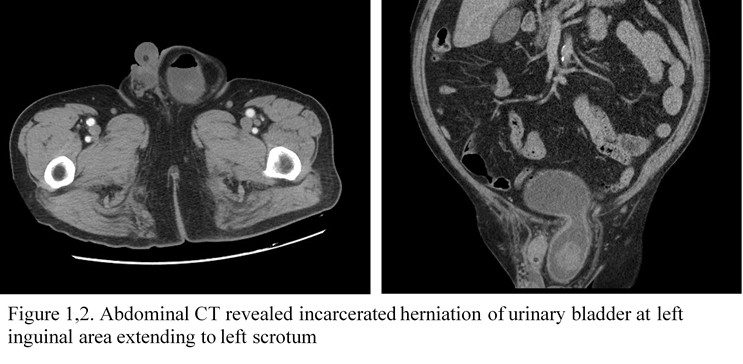
The operation then convert to transurethral blood clot evacuation after hernia repair. Prostate oozing was noted, blood clot evacuation and hemostasis were done. One bladder diverticulum noted on left lateral aspect of bladder (Figure 6).
Post-operative recovery was uneventful, smooth voiding after Foley removal. Patient was discharged asymptomatic regarding urination 6 days after operation.
Discussion
We report a rare case post-TURP complication, a left-sided inguinal hernia with bladder diverticulum herniation resulted from acute urinary retention caused by blood clot obstruction. Inguinal bladder hernia was first described by Levine in 1951 [7] as a scrotal cystocele. Inguinal bladder hernias mostly occur in patients aged over 50 years [9]. Weakening of the bladder tone and supporting structures have been hypothesized to contribute to bladder herniation. Conditions like bladder-outlet obstruction (benign prostate hyperplasia, bladder neck strictures), chronically distended bladder, decreased bladder tone, direct inguinal hernia, male gender, obesity and weakness of abdominopelvic wall are the most known etiopathological factors [8, 10]. Usually there is bladder-outlet obstruction which leads to bladder distention. In combination with weakening of abdominal and bladder wall the bladder slides through dilated inguinal ring [13].
Small inguinal bladder hernia is usually asymptomatic. Large inguinal bladder hernia usually presents with swelling in the inguinoscrotal area and lower urinary tract symptoms that results from bladder obstruction or infection. Inguinal bladder hernia may also present with two-stage voiding [8]. The first stage involves natural bladder emptying and the second stage is achieved by manual compression of the hernia [8, 10].
Most inguinal bladder hernias are diagnosed intraoperatively, 7% preoperatively and 16% postoperatively due to complications [10, 14]. Ultrasonography is the first and most accessible diagnostic modality. It demonstrates hypoechoic mass lesion protruding from the bladder. Voiding cystourethrography is the best diagnostic imaging modality which may reveal dog-ear shaped bladder in the hernia [8]. CT is indicated in obese males, aged over 50 years, with inguinal swelling and lower urinary tract symptoms [10]. Other urologic modalities such as flexible cystoscopy in indicated for confirming the diagnosis, also for evaluation of prostate and bladder conditions. If gross hematuria is present, cystoscopy is indicated to exclude additional pathology of the bladder. Inguinal bladder hernia may be mistaken for bladder diverticulum due to radiological and cystoscopic appearance [14]. A correct preoperative diagnosis may be helpful to avoid iatrogenic bladder injury. A CT scan of the case presented above was sufficient to make correct diagnosis.
The standard treatment of inguinal bladder hernias is the surgical repair with a mesh to prevent recurrence. The herniated bladder is resected and/or reduced from hernia sac and repositioned in its anatomical position [8, 14]. Indications for bladder resection are bladder damage during hernioplasty, necrosis of bladder neck, bladder tumors, bladder diverticulum and hernia neck of less than 5 mm in diameter [8, 10, 14]. Damage of bladder during hernioplasty is common and as high as 12% in inguinal bladder hernias [10, 14]. The rate drops when inguinal bladder hernia is diagnosed preoperatively [10].
Conclusion
Inguinal hernias with urinary bladder herniation is a rare condition. They are often difficult to diagnose and should be considered in obsess males, aged over 50 years with LUTS. Preoperative imaging is essential for correct diagnosis and prevention of iatrogenic injury. Bladder should be inspected for damages and should be repaired. Partial resection of the bladder in only recommenced if bladder wall necrosis or bladder diverticulum is evident. An open surgical repair with mesh by Lichtenstein technique is the standard management.
References
1. Kingsnorth, A. and K. LeBlanc, Hernias: inguinal and incisional. Lancet, 2003. 362(9395): p. 1561-71.
2. Khan, A., et al., Laparoscopic repair of massive inguinal hernia containing the urinary bladder. Urol Ann, 2014. 6(2): p. 159-62.
3. Cybulka, B., et al., Surgical Trap of a Routine Procedure. Scrotal Hernia with Concomitant Sliding of the Urinary Bladder--Case Report. Pol Przegl Chir, 2015. 87(11): p. 587-91.
4. Taskovska M, J.J., Inguinal hernia containing urinary bladder-A case report. Int J Surg Case Rep., 2017. 2017(49): p. 36-38.
5. Vasiliki Papatheofani, K.B., and Natascha C. Nuessler, Inguinal hernia with complete urinary bladder herniation: a case report and review of the literature. Journal of Surgical Case Reports, 2020. 1: p. 1-2.
6. Trobs, R.B., et al., Direct bladder hernia after indirect hernia repair in extremely low birth weight babies: two case reports and a review of the literature. J Med Case Rep, 2017. 11(1): p. 15.
7. Levine, B., Scrotal cystocele. J Am Med Assoc, 1951. 147(15): p. 1439-41.
8. Hamidi Madani A, M.N.H., Baghani Aval H, Enshaei A, Asadollahzade A, Esmaeili S, Scrotal herniation of bladder: a case rerport. Iran J Med Sci, 2013. Mar; 38(1): p. 62-4.
9. Mohan, A. and K. Srinivasan, Scrotal Cystocele in a Sliding Left Inguinoscrotal Hernia: A Case Report and Review of Literature. Euroasian J Hepatogastroenterol, 2017. 7(1): p. 87-88.
10. Moufid, K., D. Touiti, and L. Mohamed, Inguinal bladder hernia: four case analyses. Rev Urol, 2013. 15(1): p. 32-6.
11. Herskowitz, M.M., J. Reid, and R.F. Leonardo, Chronic Dialysis Dependent Renal Failure Resulting from a Massive Bladder Containing Inguinal Hernia. Case Rep Radiol, 2017. 2017: p. 2368237.
12. Habib, A., A Rare Case of Inguinal Hernia with Complete Bladder Herniation. Case Rep Surg, 2017. 2017: p. 4658169.
13. Guo Liang Yong, M.Y.S., Amelia Jia Ling Yeoh, George Eng Geap Lee, Inguinal Bladder Hernia: Case Report. Open Journal of UROLOGY, 2013. 3(5).
14. Kraft, K.H., et al., Inguinoscrotal bladder hernias: report of a series and review of the literature. Can Urol Assoc J, 2008. 2(6): p. 619-23.