男性在攝影尿動力學逼尿肌活動力不足的新分類
翁慧鈴1、郭漢崇2
大林慈濟醫院 外科部 泌尿科;1花蓮慈濟醫院 泌尿部.2
A new classification of detrusor underactivity based on videourodynamic characteristics in men.
Hueih Ling Ong 1, Hann-Chorng Kuo 2.
1Department of Urology, Dalin Tzu Chi General Hospital and Buddhist Tzu Chi Medical Foundation, Chia-Yi, Taiwan
2Department of Urology, Buddhist Tzu Chi General Hospital and Tzu Chi University, Hualien, Taiwan
Purpose:
Detrusor underactivity (DU) is abridged from low detrusor pressure, poor sustainability, and poor flow rate [1]. DU may result from impaired detrusor contractility, sensory afferent pathway, central nervous system and motor efferent nerves [2]. The variation of low detrusor contractility associated with delayed opening of bladder neck while voiding, early termination of voiding, reduced bladder sensation at filling phase, detrusor acontractile, or with detrusor overactivity were all diagnosed as DU. The lack of effective therapy may relate to both etiologic and diagnostic uncertainty due to terminological imprecision. This study is aimed to identify the diversity characteristics of DU based on videourodynamics (VUDS).
Materials and Methods:
A retrospective observation study performed from April 1988 to August 2010. Male patients with clinical presentation of dysuria, urinary retention and large post-void residual volume (PVR) undergone VUDS. Patients with urinary tract infection, genitourinary tract malignancy, myelomeningocele and multiple sclerosis, bladder contractility index (BCI) ≥ 100 were excluded from the study. Those who diagnosed with DU from, were enrolled into this study. The study divided patients into 2 groups according to detrusor pressure at maximal flow (Pdet): low detrusor contractility (LDC) 6≤ Pdet≤40 cmH20; detrusor acontractility (DA) Pdet ≤5cmH20. The parameters of VUDS were analyzed between 2 groups and compared with normal bladder group.
Results:
A total of 298 men were enrolled into the study, 151 patients in LDC group, and 147 patients in DA group. DA patients had lower Pdet, abdominal pressure (Pabd), maximal flow rate (Qmax), voided volume (Vol.), BCI and bladder outlet index (BOOI), p=0. But higher cystometric bladder capacity (CBC), first sensation of filling (FSF), bladder full sensation (FS), and PVR. Patients with LDC had higher incidence of detrusor overactivity (DO), 35.3% vs.5.3%, p=0; and lower incidence of bladder neck narrowing in VUDS during voiding phase, 31.8%% vs. 46.9%, p=0.007. Among patients with LDC with DO, a lower CBC (p=0) and older in age (p=0.002) were indicated, but a higher Pdet (p=0.014) was indicated. However, Qmax, Vol. and PVR showed no significant difference. Comorbidity such as cerebrovascular disease, dementia, Parkinsonism, Diabetes Mellitus and chronic renal failure showed no significant between groups.
Conclusion:
Bladder filling sensation and BCI were crucial to distinguish the severity of DU. A new precise classification of DU may develop a more accurate diagnostic criteria. It is crucial for further research on the underlying pathophysiology of this disease, so that a better treatment may develop within sight.
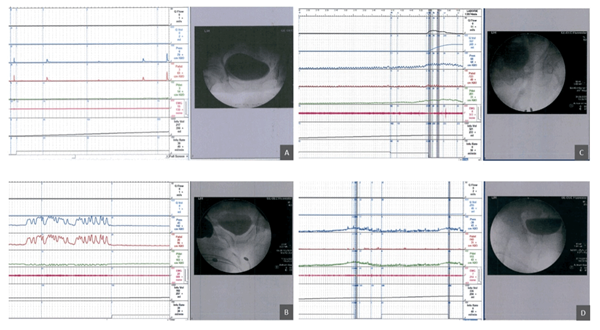
Figure 1: The videourodynamic differentiation of detrusor underactivity. (A) Acontractile detrusor. (B) Low detrusor contractility. (C) Low detrusor contractility with delayed initiation. (D) Low detrusor contractility with low sustainability.
|
|
DA (n=147) |
LDC (n=151) |
Normal (n=30) |
|
Age |
70.91±13.70 |
71.50±13.22 |
69.73±5.10 |
|
CBC |
351.16±131.66* |
311.01±140.66# |
403.57±123.44 |
|
FSF/CBC (%) |
63.27±23.27*# |
55.91±18.52# |
46.14±15.38 |
|
FS/CBC (%) |
87.84±16.18# |
85.13±15.12# |
75.72±13.50 |
|
US/CBC (%) |
99.11±5.01 |
98.77±4.77 |
97.02±6.91 |
|
PVR/CBC (%) |
114.67±80.92# |
91.50±92.58# |
4.00±5.46 |
|
Pves |
31.14±35.86# |
36.49±26.32 |
50.39±30.53 |
|
Pabd |
29.82±36.01* |
18.22±26.54 |
17.61±25.95 |
|
Pdet |
1.31±2.07*# |
18.27±9.32# |
32.60±12.64# |
|
Qmax |
1.13±2.78*# |
3.34±3.61# |
20.10±3.10 |
|
Vol. |
32.25±85.52*# |
85.31±108.29# |
484.87±102.80 |
|
Compliance |
70.88±104.51 |
65.24±85.44 |
68.21±57.29 |
|
BCI |
6.98±14.35*# |
34.99±21.01# |
133.10±22.85# |
|
BOOI |
-0.95±5.65*# |
11.58±11.30# |
-7.60±12.23 |
DA
DA: Acontractile detrusor; LDC: Low detrusor contractility; CBC: cystometric bladder capacity; FSF: first sensation of filling; FS: full sensation; US: urge sensation; PVR: post-void residual volume; Pves: intravesical pressure; Pabd: abdominal pressure; Pdet: detrusor pressure at Qmax; Qmax: maximum flow rate; BCI: Bladder Contractility Index; BOOI: Bladder outlet index. *P<0.05 compared with the LDC;#P<0.05 compared with control.
: Acontractile detrusor; LDC: Low detrusor contractility; CBC: cystometr