女性急性膀胱炎症狀與如廁後灌洗習慣之臨床特徵及差異
張建偉1、姜秉均1
1財團法人天主教新店耕莘醫院醫學研究中心暨天主教輔仁大學醫學院
Differences in Clinical Characteristics Between Acute Cystitis Symptoms in Women with and without Irrigation Habits After Toilet Use
Kian-Woei Chong1、 Bing-Juin Chiang1
1Medical Research Center, Cardinal Tien Hospital and School of Medicine, College of Medicine, Fu Jen Catholic University, New Taipei City 231, Taiwan
Abstract: Acute cystitis is common, especially in females. In clinical practice, we have found that female patients with lower urinary tract symptoms, including dysuria and urinary frequency, particularly those with the habit of irrigation after using the toilet, require a longer course of antibiotic treatment than those without this habit. Irrigation after using the toilet is becoming increasingly popular in Asian countries, such as Japan, Taiwan, and Indonesia, due to the use of bidet toilets. This study was conducted between October 2021 and September 2022 at Cardinal Tien Hospital in Taipei City, Taiwan, to investigate the relationship between acute cystitis and irrigation after using the toilet.
Introduction: The practice of washing or irrigating the anal or urogenital area after defecation, urination, or during menstruation is becoming increasingly popular since the invention of electronic bidet toilets, especially in Japan, Taiwan, China, and even Western countries. E. coli is a common gut bacteria that can cause urinary tract infections (UTIs) when it colonizes the urogenital tract. In females, the anus is in close proximity to the genitalia and the urethra. One proposed mechanism for the colonization of the urogenital tract with E. coli is the way in which a woman wipes herself after using the toilet. Wiping from back to front could potentially bring E. coli forward from the perianal area to the urethra, thereby increasing the risk of bacterial colonization and UTIs. In contrast, women who wipe from front to back may have reduced colonization and therefore a lower incidence of UTIs or asymptomatic bacteriuria. Therefore, using irrigation (including electronic bidet or manual irrigation) is assumed to have the same mechanism of bacterial colonization of the urogenital tract. Our study aims to investigate the relationship between acute cystitis and irrigation after using the toilet in females.
Material and method: A total of 823 women with suspected acute cystitis who presented at the outpatient clinics of Cardinal Tien Hospital in Taipei City, Taiwan between October 2021 and September 2022 were retrospectively recruited. Individuals were included if they were female and had a documented history of lower urinary tract symptoms, including urinary frequency and dysuria. The exclusion criteria were patients aged less than 20 years old, those with functional or anatomical abnormalities of the genitourinary tract, neurogenic bladder, interstitial cystitis, asymptomatic bacteriuria, an indwelling urinary catheter, hormone replacement therapy, urinary tract tumors, pregnancy, or complicated urinary tract infection. Collected information included age, sex, comorbidity, antibiotic use, duration of antibiotic use, urine analysis, urine culture result and sensitivity, and habits of using irrigation after using the toilet. In total, 35 cases and 98 controls were included in the final analysis.
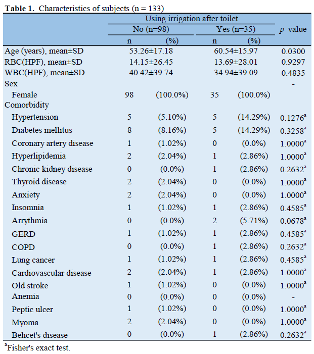
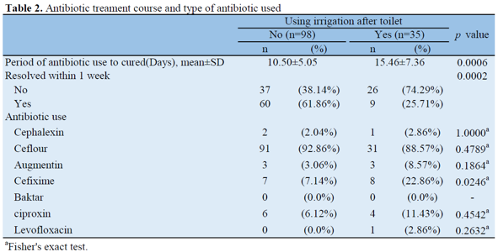
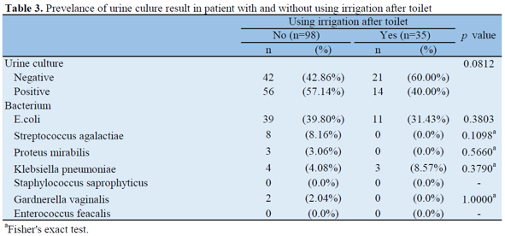
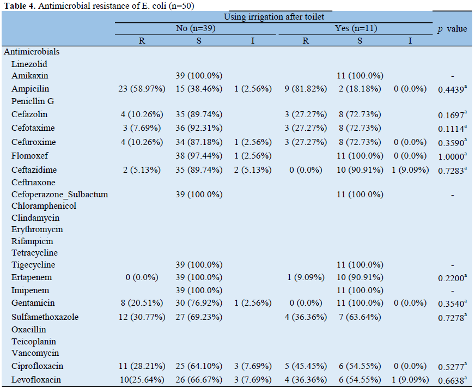
Results: The characteristics of the analyzed subjects are shown in Table 1. The mean age of the control group was 53.26±17.18 years, and that of the cases was 60.54±15.97 years, with a significant difference (p value=0.03) in age between the cases and controls groups. There was a prevalence of elderly individuals favoring the use of irrigation after using the toilet. There was no significant difference in comorbidity between the two groups. In Table 2, the mean duration of antibiotic use to cure the infection in the control group was 10.50±5.05 days, and that in the cases was 15.46±7.36 days, which was significantly higher in the cases than the control group (p=0.006). The percentage of cases where symptoms resolved within one week after antibiotic treatment was significantly higher in the control group (61.86%) than in the cases group (25.71%, p=0.0002). There was no significant difference in the urine culture positive rate between the control and cases groups (57.14% vs. 40.0%, p=0.0812). The urine culture bacterium showed that the control group had a slightly higher culture rate with E.coli (39.80% vs. 31.43%, p=0.3803), and the cases group had a slightly higher culture rate with Klebsiella pneumoniae (4.08% vs. 8.57%, p=0.3790), but these differences did not reach statistical significance, as shown in Table 3. There were no significant differences in the antimicrobial resistance test of E.coli in both groups, as shown in Table 4.
Discussion: Using irrigation after toilet use was associated with an increase in the period of antibiotic use to cure UTIs and a decrease in the rate of resolution within one week. This suggests that patients who use irrigation after toilet might need to use antibiotics longer than those who do not. In our study, the majority of patients had lower urinary tract symptoms caused by E. coli, which is a common cause of UTIs that can ascend the urinary tract and lead to more severe infections such as cystitis or pyelonephritis. There are several limitations to our study. Firstly, wiping from back to front is associated with an increase in colonization and therefore an increase in the incidence of UTI or asymptomatic bacteriuria, but we did not consider the patients' wiping habits after using the toilet. Secondly, we did not take into consideration the method of irrigation after toilet, frequency, time of using a bidet toilet, or the water jet pressure in our survey. Thirdly, comparing patients who cease using irrigation after toilet with those who continue to use it might help identify this relationship. Lastly, our sample size was relatively small (n = 133), and larger samples are needed to more closely approximate the population and improve the power of the study to draw conclusions.
Conclusion: Based on the results of the study, using irrigation after toilet use was associated with an increase in the period of antibiotic use to cure UTIs and a decrease in the rate of resolution within one week. This suggests that patients who use irrigation after toilet might need to use antibiotics longer than those who do not. However, there are several limitations to the study, including the relatively small sample size, lack of consideration of wiping habits and irrigation method details, and the need for larger samples to draw more accurate conclusions. Therefore, further research is needed to determine the exact relationship between using irrigation after toilet and UTI treatment outcomes.
References:
- Inoue K. IT media executive. Available at http://mag.executive.itmedia.co.jp/executive/articles/1303/13/new
s012.html (Accessed 20 September 2017) (in Japanese).
- Asakura K, et al. (2013) Effect of bidet toilet use on preterm birth and vaginal flora in pregnant women. Obstetrics and Gynecology 121, 1187–1194.
- Kiuchi T, et al. (2017) Bidet toilet use and incidence of hemorrhoids or urogenital infections: a one-year follow-up web survey. Preventive Medicine Reports 6, 121–125.
- Ogino M, Iino K and Minoura S (2010) Habitual use of warm-water cleaning toilets is related to the aggravation of vaginal microflora. The Journal of Obstetrics and Gynaecology Research 36, 1071–1074.
- Tsunoda A, et al. (2016) Survey of electric bidet toilet use among community dwelling Japanese people and correlates for an itch on the anus. Environmental Health and Preventive Medicine 21, 547–553.
- Kohdaira T (2009) Correlation of recurrent cystitis and using of toilet seat with shower unit. Japanese Journal of Urological Surgery 22, 1217–1222.
- L.E. Nicolle, G.K.M. Harding, J. Preiksaitis, A.R. Ronald The association of urinary tract infection with sexual intercourse J Infect Dis, 146 (1982), pp. 579-583.
- R.R. Remis, M.J. Gurwith, D. Gurwith, N.T. Hargrett-Bean, P.M. Layde Risk factors for urinary tract infection Am J Epidemiol, 126 (1987), pp. 685-694.
- K. Adatto, K.G. Doebele, L. Galland, L. Granowetter Behavioral factors and urinary tract infection JAMA, 241 (1979), pp. 2525-2526.
- B. Foxman, R.R. Frerichs Epidemiology of urinary tract infection: 11. Diet, clothing and urination habits Am J Public Health, 75 (1985), pp. 1314-1317.
- T.A. Stamey, M. Timothy, M. Millar, et al. Recurrent urinary infections in adult women: the role of introital bacteria Calif Med, 115 (1971), pp. 1-19
- C.M. Kunin, F. Polyak, E. Postel Periurethral bacterial flora in women: prolonged intermittent colonization with Escherichia coli JAMA, 243 (1980), pp. 134-139
- A. Kilmartin Cystitis: the Complete Self-help Guide Warner Brooks, New York (1980)
- B. Foxman Recurring lower urinary tract infections: occurrence and determinants Am J Public Health (1990) in press
- Foxman B, Chi JW. Health behavior and urinary tract infection in college-aged women. J Clin Epidemiol. 1990;43(4):329-37. doi: 10.1016/0895-4356(90)90119-a. PMID: 2324774.
- Yazdi S, Alidousti K, Tirgari B, Jahani Y. Effect of integrated health promotion intervention and follow up on health issues (clothing way, food habits, urinary habits, sexual behavior habits) related to urinary tract infection among pregnant women. A randomized, clinical trial. J Prev Med Hyg. 2020 Jul 4;61(2):E194-E199 doi: 10.15167/2421-4248/jpmh2020.61.2.1412. PMID: 32803005; PMCID: PMC7419116.